WHAT IS MACULAR EDEMA SECONDARY TO INFLAMMATION (MESI)?
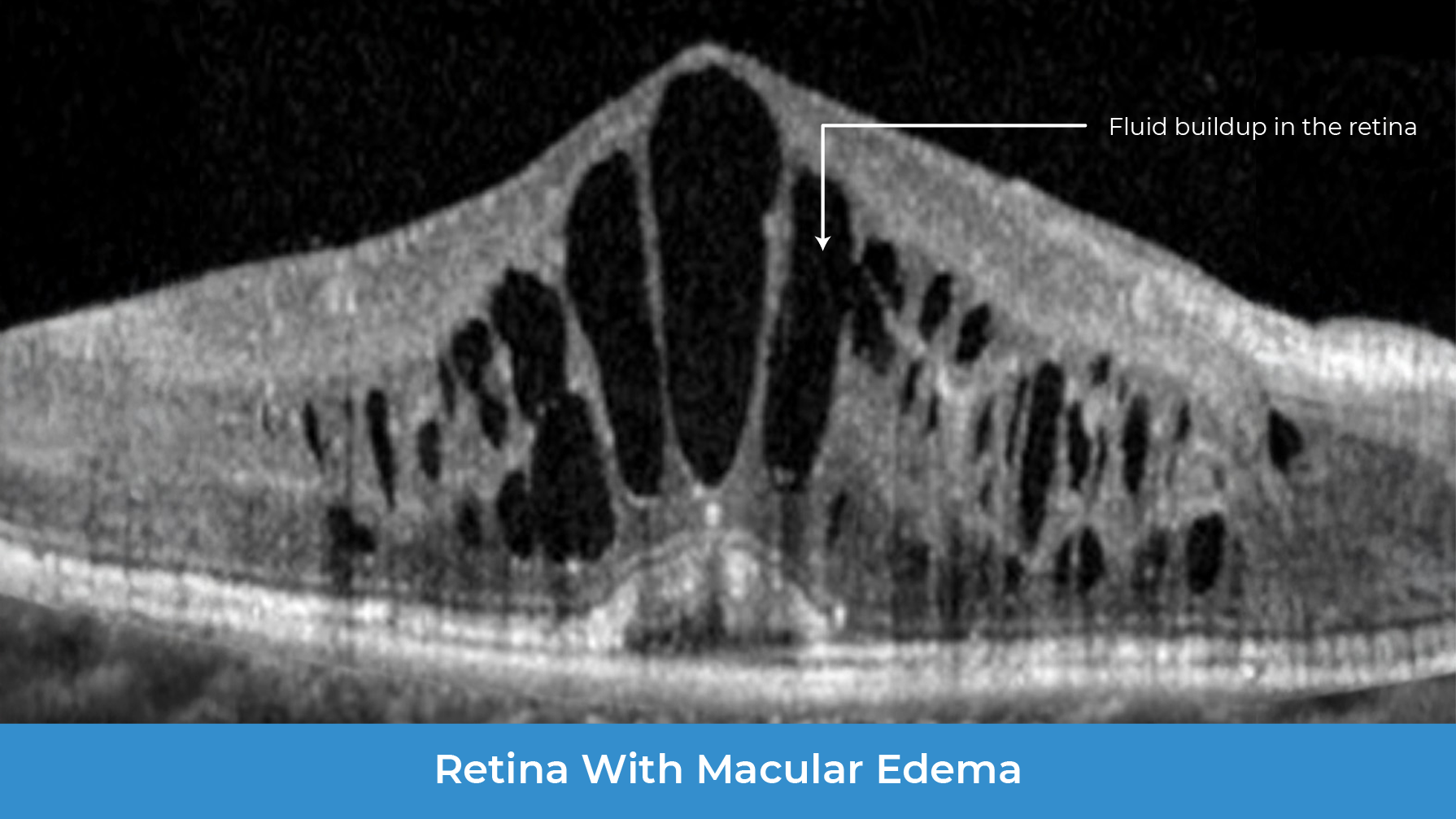
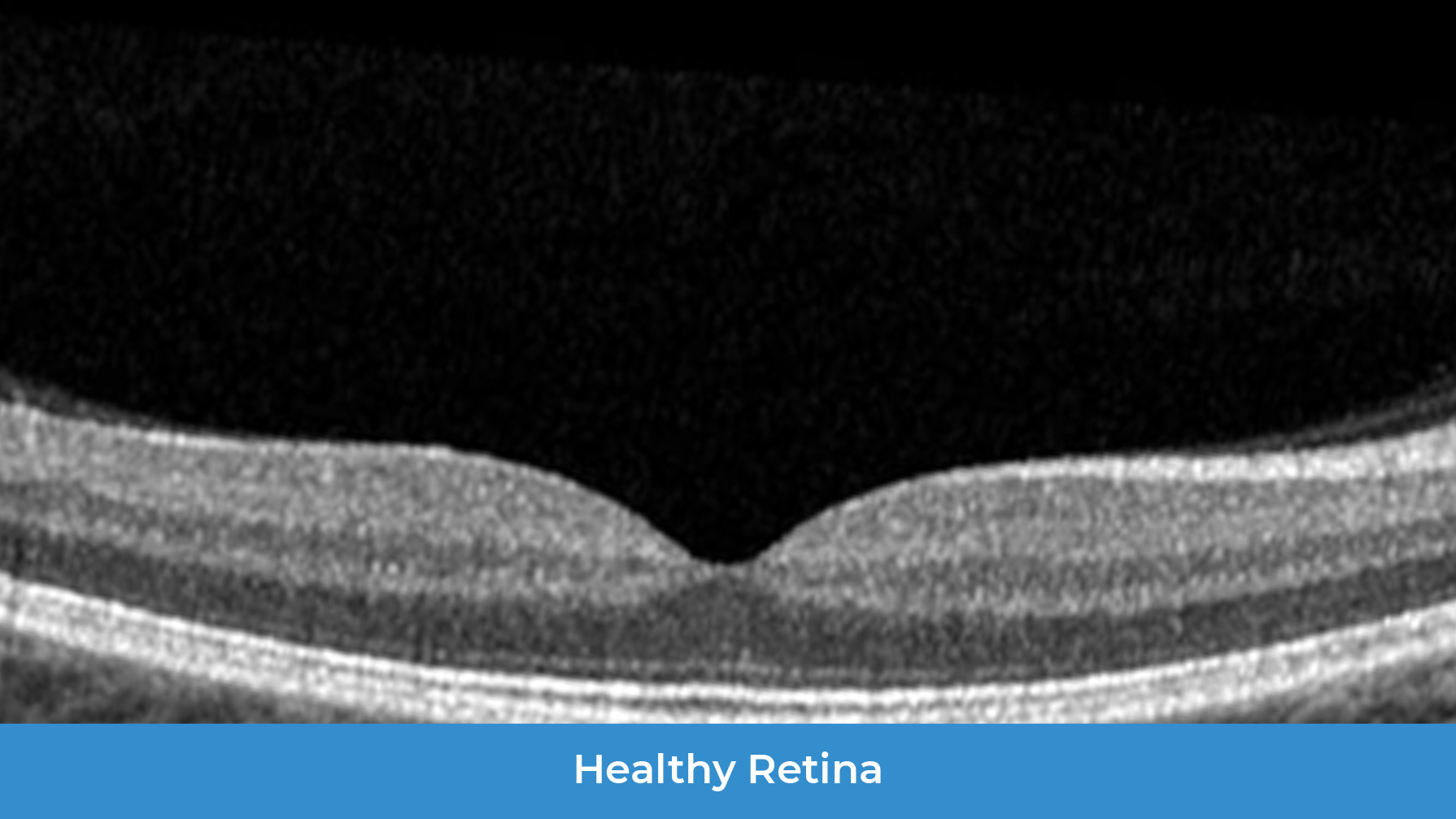
Macular edema secondary to inflammation (MESI) is a group of inflammatory diseases that cause swelling (edema) in the macula, the part of the retina responsible for sharp, central vision. This swelling occurs when inflammation – past or present – causes fluid to build up in the macula which can lead to blurry or distorted central vision. If not treated effectively, MESI can result in significant vision loss.
Many diseases can cause inflammation inside the eye leading to MESI:
Autoimmune
Conditions
Systemic
Autoimmune
Conditions
Such as ankylosing spondylitis, juvenile
idiopathic arthritis and multiple
sclerosis.
These diseases can trigger an immune
response in the eye.
Conditions
Localized to
the Eye
Autoimmune Conditions Localized
to the Eye
Such as serpiginous choroidopathy and
multifocal choroiditis
Post-Procedural
Such as after vitrectomy, cataract and
glaucoma surgery
Unknown
In many cases, the exact cause of MESI
is unknown
Regardless of the cause, all patients with MESI share the same clinical feature:
macular edema with visual impairment
HOW DOES MESI DIFFER FROM OTHER EYE DISEASES THAT CAUSE MACULAR EDEMA?
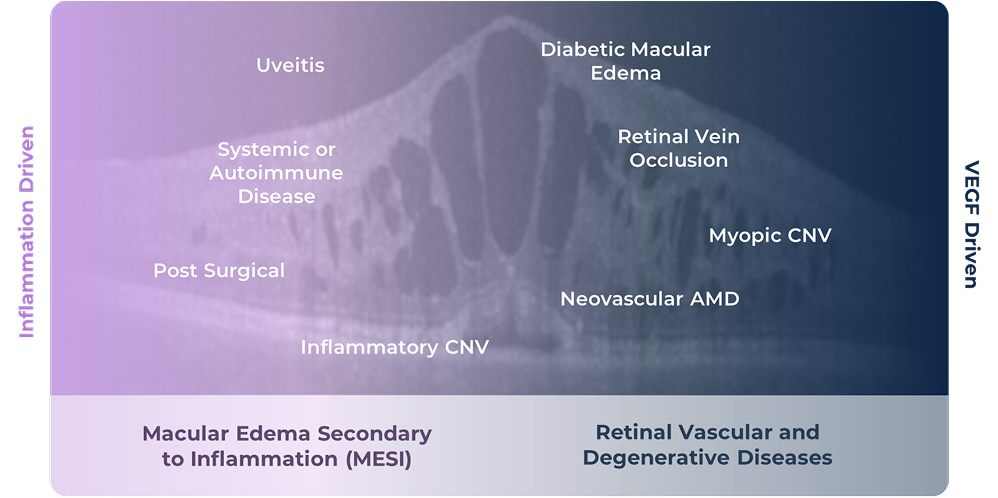
Macular edema is a common feature seen in a wide spectrum of eye diseases. It can be driven by inflammation inside the eye, by elevated levels of a protein called VEGF, or by both working together. In MESI, inflammation is the primary driver of disease, and VEGF also plays an important role and contributes to the swelling.
The spectrum of diseases that present with macular edema:
WHAT CAUSES MESI?
MESI occurs when an immune trigger (such as an autoimmune disease) causes a complex response in the eye that damages the blood-retinal barrier, the filter that normally protects the retina. Once this barrier is disrupted, blood factors and fluid can leak into the retina, causing inflammation, leakage and macular edema.
In MESI, two proteins – IL-6 and VEGF – are co-induced in high amounts. These proteins interact with each other and work together to weaken the blood-retinal barrier. IL-6 keeps the eye inflamed and also increases VEGF levels. VEGF, in turn, makes the blood vessels fragile and leaky. Acting together, they cause more damage than either one alone, making it easier for blood factors and fluid to leak into the macula and cause swelling.
CURRENT TREATMENT AND LIMITATIONS
Steroids are the most common treatment for MESI. They can help reduce inflammation and swelling, but when used at high doses or for long periods they can cause serious side effects in the eye, including glaucoma and cataracts that require surgery. Because of this, steroids are used cautiously in adults and avoided in children. Around 30–40% of patients also do not respond fully to steroid treatment in the eye.
Systemic therapies may also be used to treat the diseases that lead to MESI. They can reduce the need for long-term steroid use but carry serious side effects that affect the whole body.
Side effects from today’s treatments often cause patients with MESI to be undertreated and underdiagnosed.
HOW KODIAK CAN HELP
There is a need for new treatments that target both disease drivers while remaining minimally invasive and safe. KSI-101 is a high-strength, locally delivered therapy designed to block both IL-6 and VEGF at the same time, with the potential to serve as a unifying treatment for all patients with MESI. Learn more









